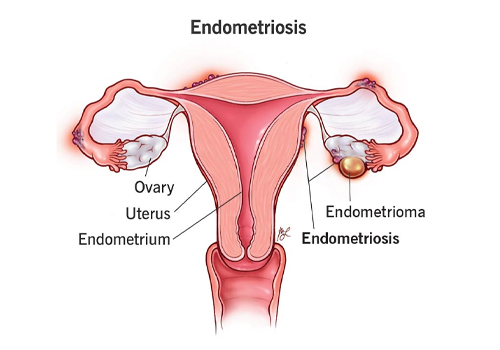
Endometriosis
Endometriosis is a chronic condition in which tissue similar to the lining inside the uterus (endometrium) grows outside the uterus. This endometrial-like tissue can be found on the ovaries, fallopian tubes, outer surface of the uterus, and other organs within the pelvic cavity. Although it is benign, it can cause significant pain and other complications.
Causes of Endometriosis:
The exact cause of endometriosis is not fully understood, but several theories exist:
- Retrograde Menstruation: Menstrual blood containing endometrial cells flows backward through the fallopian tubes into the pelvic cavity instead of leaving the body.
- Embryonic Cell Transformation: Hormones like estrogen may transform embryonic cells (cells present since birth) into endometrial-like cell implants during puberty.
- Surgical Scars: After surgeries such as a cesarean section, endometrial cells may attach to the incision site.
- Immune System Disorders: A malfunctioning immune system may fail to recognize and destroy endometrial-like tissue growing outside the uterus.
- Genetics: Endometriosis may run in families, suggesting a genetic predisposition.
Symptoms of Endometriosis:
-
Pelvic Pain:
- Dysmenorrhea (painful periods): Pain before and during menstruation, often severe and disabling.
- Chronic pelvic pain: Constant or intermittent pain in the lower abdomen, pelvis, or lower back.
-
Pain During Intercourse:
- Pain during or after sex (dyspareunia) is common, especially with deep penetration.
-
Heavy Menstrual Bleeding:
- Some women with endometriosis experience heavy periods (menorrhagia) or bleeding between periods.
-
Infertility:
- Endometriosis is often found in women seeking treatment for infertility. It can affect fertility by causing scar tissue (adhesions), blockages, or structural abnormalities of the reproductive organs.
-
Pain with Bowel Movements or Urination:
- Pain during bowel movements or urination, especially during menstruation, may be a symptom.
-
Fatigue, Diarrhea, Constipation, and Bloating:
- Other symptoms may include gastrointestinal issues, especially during menstruation.
Diagnosis of Endometriosis:
Diagnosing endometriosis can be challenging as symptoms overlap with other conditions. Methods include:
-
Medical History and Physical Examination:
- A detailed history of symptoms, menstrual patterns, and family history of endometriosis.
- A pelvic exam can sometimes reveal abnormalities, but small lesions may not be detectable this way.
-
Imaging Tests:
- Ultrasound: While it can't definitively diagnose endometriosis, it can help identify cysts (endometriomas) associated with the condition.
- Magnetic Resonance Imaging (MRI): Provides detailed images of the reproductive organs and may help in surgical planning.
-
Laparoscopy (Gold Standard for Diagnosis):
- A minimally invasive surgical procedure where a thin, lighted tube (laparoscope) is inserted through a small incision in the abdomen to view and potentially remove endometrial tissue.
- Biopsy of suspicious tissue can confirm the diagnosis.
Stages of Endometriosis:
Endometriosis is classified into four stages (minimal to severe), based on the location, depth, and extent of the implants, as well as the presence of scar tissue:
- Stage 1 (Minimal): Small, superficial lesions and no significant scarring.
- Stage 2 (Mild): More lesions, deeper involvement, and small areas of scarring.
- Stage 3 (Moderate): Numerous deep implants, with small cysts on the ovaries and thick adhesions.
- Stage 4 (Severe): Large implants, deep lesions, multiple cysts on the ovaries, and dense adhesions.
Treatment of Endometriosis:
Treatment depends on the severity of symptoms, the extent of the disease, and a woman's desire for future fertility.
-
Medications:
- Pain relievers: Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can help manage pain.
- Hormonal Therapies:
- Birth control pills, patches, or vaginal rings can help control the growth of endometrial-like tissue and reduce pain.
- GnRH agonists (e.g., Lupron) induce temporary menopause by lowering estrogen levels, which can shrink lesions.
- Progestins: Hormones that can stop menstruation and reduce the growth of endometrial tissue.
- Aromatase inhibitors: These drugs lower estrogen levels and may be used in conjunction with other treatments.
-
Surgical Treatment:
- Laparoscopic Excision: During diagnostic laparoscopy, endometrial implants and scar tissue can be removed or burned away. This procedure can relieve symptoms and improve fertility.
- Hysterectomy: In severe cases, removal of the uterus and possibly the ovaries (oophorectomy) may be recommended, especially if other treatments fail. This is typically a last resort for women who do not plan to have more children.
-
Fertility Treatments:
- Women with endometriosis who are struggling to conceive may benefit from in vitro fertilization (IVF) or other assisted reproductive technologies (ART).
-
Lifestyle and Complementary Therapies:
- Diet and exercise: A balanced diet rich in anti-inflammatory foods, regular physical activity, and maintaining a healthy weight may help manage symptoms.
- Stress management: Practices like yoga, meditation, and acupuncture may reduce pain and improve quality of life.
- Heat therapy: Applying heat (e.g., heating pads) to the lower abdomen can help alleviate pain.
Impact of Endometriosis on Fertility:
- Endometriosis can cause structural damage to the ovaries or fallopian tubes, affecting fertility.
- Adhesions and scar tissue may block the passage of the egg or disrupt the function of reproductive organs.
- Treatment through surgery to remove lesions can improve fertility in some cases.
- Women with milder stages of endometriosis may still conceive naturally or with the help of fertility treatments.
When to Seek Medical Help:
- If you experience severe pelvic pain, particularly around your menstrual cycle.
- If you have difficulty becoming pregnant after trying for 6 months to a year.
- If over-the-counter pain medications do not relieve symptoms.
- For abnormal bleeding, including heavy periods or bleeding between periods.