Uterning Fibroids and Polyps
Uterine Fibroids and Uterine Polyps are two common benign (non-cancerous) growths that affect women, particularly during their reproductive years and around the time of menopause. Though both can cause similar symptoms, they are distinct in their nature, location, and treatment options.
Uterine Fibroids (Leiomyomas)
What Are Fibroids?
Uterine fibroids are benign tumors that develop from the smooth muscle tissue of the uterus (myometrium). They can vary in size, from as small as a seed to as large as a grapefruit, and may occur singly or in clusters.
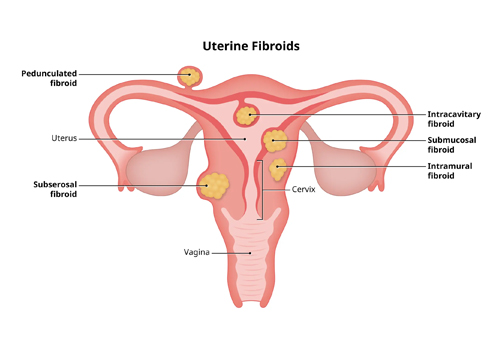
Types of Fibroids:
-
Intramural Fibroids:
- Located within the muscular wall of the uterus.
- The most common type of fibroid, often leading to heavy menstrual bleeding and pelvic pain.
-
Subserosal Fibroids:
- Develop on the outer wall of the uterus.
- May press on surrounding organs like the bladder or intestines, causing pressure or bloating.
-
Submucosal Fibroids:
- Found just beneath the lining of the uterine cavity.
- Often cause significant menstrual bleeding and can interfere with fertility.
-
Pedunculated Fibroids:
- Grow on a stalk either outside or inside the uterus, resembling a mushroom.
- Can cause pain if the stalk twists.
Symptoms of Uterine Fibroids:
- Heavy or prolonged menstrual periods (menorrhagia), sometimes with clots.
- Pelvic pressure or pain, particularly if the fibroid presses on nearby organs.
- Frequent urination or difficulty emptying the bladder (due to pressure on the bladder).
- Constipation (if fibroids press on the rectum).
- Lower back or leg pain (if large fibroids press on nerves).
- Pain during intercourse (dyspareunia).
- Enlarged abdomen or bloating.
- Fertility problems or pregnancy complications, such as miscarriage or preterm labor (in some cases).
Diagnosis of Fibroids:
- Pelvic Examination: Often, fibroids can be felt during a routine pelvic exam.
- Ultrasound: This imaging test confirms the size, location, and number of fibroids.
- MRI: May be used in complex cases to get a detailed view of fibroids.
- Hysteroscopy: A procedure in which a thin, lighted tube is inserted through the cervix into the uterus to inspect the uterine cavity and possibly remove fibroids.
Treatment Options for Fibroids:
-
Medications:
- Hormonal treatments: Birth control pills or hormonal IUDs can help control heavy bleeding but don't shrink fibroids.
- GnRH agonists: These drugs temporarily shrink fibroids by blocking estrogen production, often used before surgery to make fibroids easier to remove.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): Help relieve pain but don't reduce fibroid size.
-
Minimally Invasive Procedures:
- Uterine artery embolization (UAE): Cuts off the blood supply to fibroids, causing them to shrink.
- Myomectomy: Surgical removal of fibroids while preserving the uterus, an option for women who want to maintain fertility.
- Hysteroscopic myomectomy: For submucosal fibroids, the fibroids are removed through the cervix using a hysteroscope.
-
Surgical Procedures:
- Hysterectomy: Complete removal of the uterus, often recommended for severe cases when other treatments fail, or when the woman no longer wishes to become pregnant.
Uterine Polyps (Endometrial Polyps)
What Are Polyps?
Uterine polyps are benign overgrowths of the endometrial tissue (the lining of the uterus). Unlike fibroids, which are made of muscle, polyps are soft tissue and are generally smaller.
Types of Uterine Polyps:
- Sessile Polyps: Broad-based polyps attached directly to the uterine wall.
- Pedunculated Polyps: Polyps that grow on a stalk, extending into the uterine cavity.
Symptoms of Uterine Polyps:
- Irregular menstrual bleeding, including spotting between periods.
- Heavy menstrual bleeding.
- Postmenopausal bleeding (any bleeding after menopause).
- Infertility or difficulty conceiving in some cases, though polyps don't always affect fertility.
Diagnosis of Uterine Polyps:
- Ultrasound: A transvaginal ultrasound can detect polyps and measure their size.
- Hysterosonography: A saline solution is injected into the uterus during an ultrasound to better visualize polyps.
- Hysteroscopy: Direct visualization of the inside of the uterus using a hysteroscope, which can also be used to remove polyps.
Treatment Options for Polyps:
- Watchful Waiting: Small polyps that cause no symptoms may resolve on their own. In postmenopausal women or women with symptoms, polyps are often removed.
- Hysteroscopic Polypectomy: Polyps can be removed through the cervix using a hysteroscope, often as an outpatient procedure.
- Medications: Hormonal treatments, such as progestins or gonadotropin-releasing hormone agonists, may help reduce symptoms temporarily, but polyps often return once treatment is stopped.
- Endometrial Ablation: This procedure destroys the uterine lining, including polyps, and is used in women who don’t plan to have more children.
Comparing Fibroids and Polyps:
| Feature |
Fibroids |
Polyps |
| Composition |
Made of muscle tissue |
Made of endometrial tissue |
| Size |
Can grow large (up to grapefruit size or larger) |
Usually smaller (up to a few centimeters) |
| Symptoms |
Heavy periods, pelvic pain, pressure on bladder |
Irregular bleeding, spotting, postmenopausal bleeding |
| Effect on Fertility |
Can cause infertility or pregnancy complications |
May cause infertility, especially large or multiple polyps |
| Diagnosis |
Ultrasound, MRI, hysteroscopy |
Ultrasound, hysterosonography, hysteroscopy |
| Treatment |
Medications, surgery (myomectomy or hysterectomy) |
Hysteroscopic removal, sometimes medications |
When to See a Doctor:
- Heavy or prolonged menstrual bleeding.
- Bleeding between periods or after intercourse.
- Pelvic pain or pressure.
- Difficulty urinating or frequent urination.
- Difficulty getting pregnant or recurrent miscarriages.
- Any bleeding after menopause.
Both uterine fibroids and polyps are manageable, and treatment options depend on symptoms, age, desire for future fertility, and overall health. Early diagnosis and treatment can help prevent complications.